Neomi Shah
@NeomiShahPhysician Scientist | 🫁, Critical Care, 😴 Medicine | Sports Fan | Vegetarian | Not Afraid to Fail or Dream Big
Similar User

@AneesaDas

@AASMmembership

@AtulMalhotra13

@aasmfoundation

@cathygo_sleep

@SleepDataNSRR

@drsleepykarin

@ReenaMehra0203

@sai_sparthamd

@OrenCohen_MD

@sfaiz212

@womeninsleep

@davidschulman

@Vaish1986

@sleepdocpa
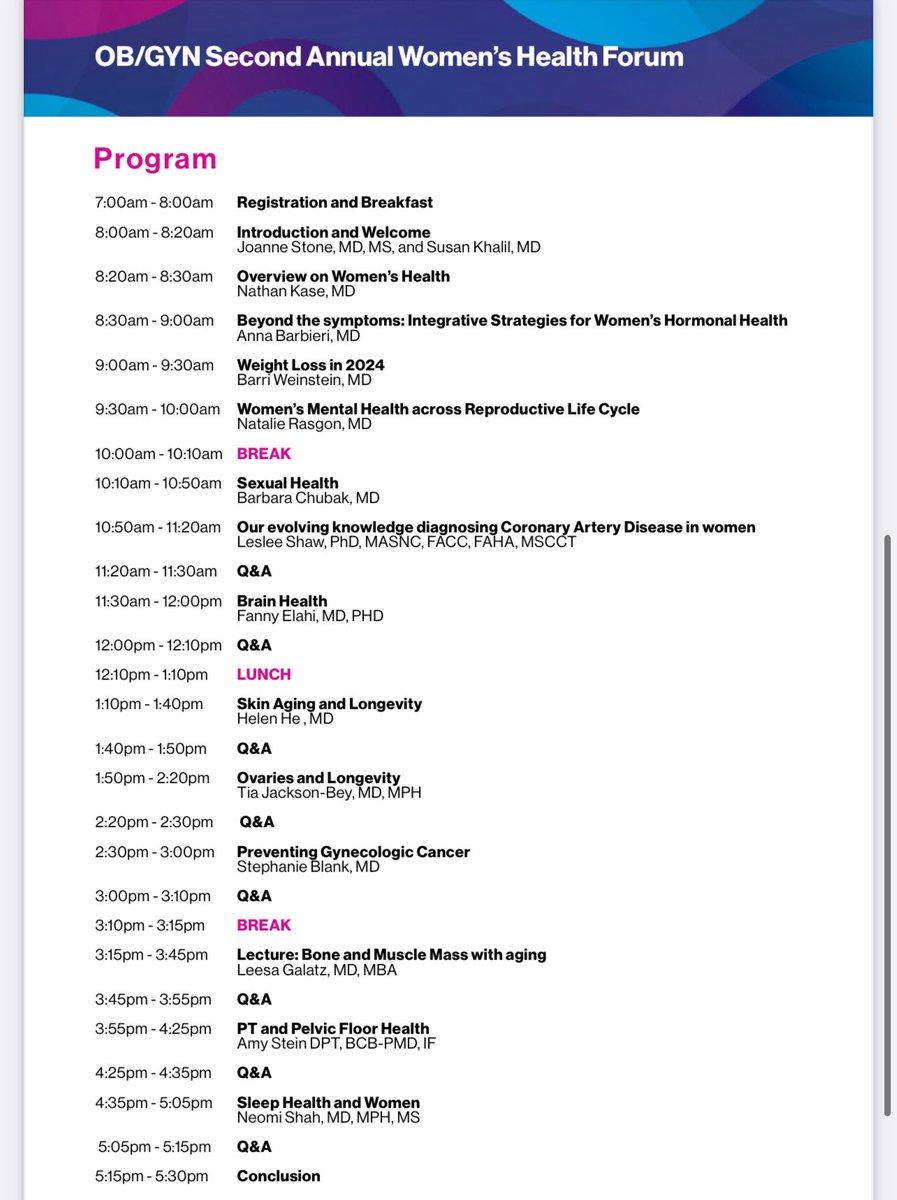
Excited to speak on Sleep and Women’s Health at the @IcahnMountSinai 2nd Annual OB/GYN Women’s Health Forum to expand knowledge, empower patients & connect with experts on women’s health. Register today! shorturl.at/KDQGZ

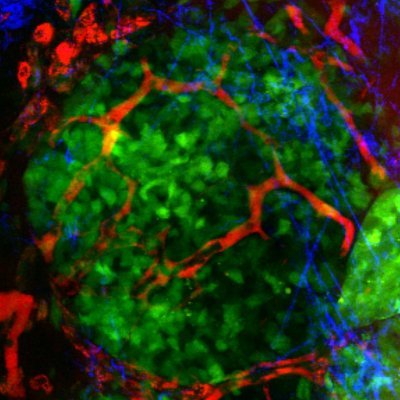
New Mount Sinai research reveals that a #HeartAttack can trigger a desire to get more #sleep, allowing the #heart to heal and reduce inflammation—and this happens because the heart sends special signals to the #brain. Learn more: mshs.co/3AmcAor @DOMSinaiNYC…
In humans, poor sleep in the weeks following STEMI or NSTEMI associates with reduced cardiac recovery and function and increases MACE+ incidence over 2 years. Further, sleep restriction in humans causes inflammatory and chemotactic reprograming of ADRβ2-responsive monocytes.
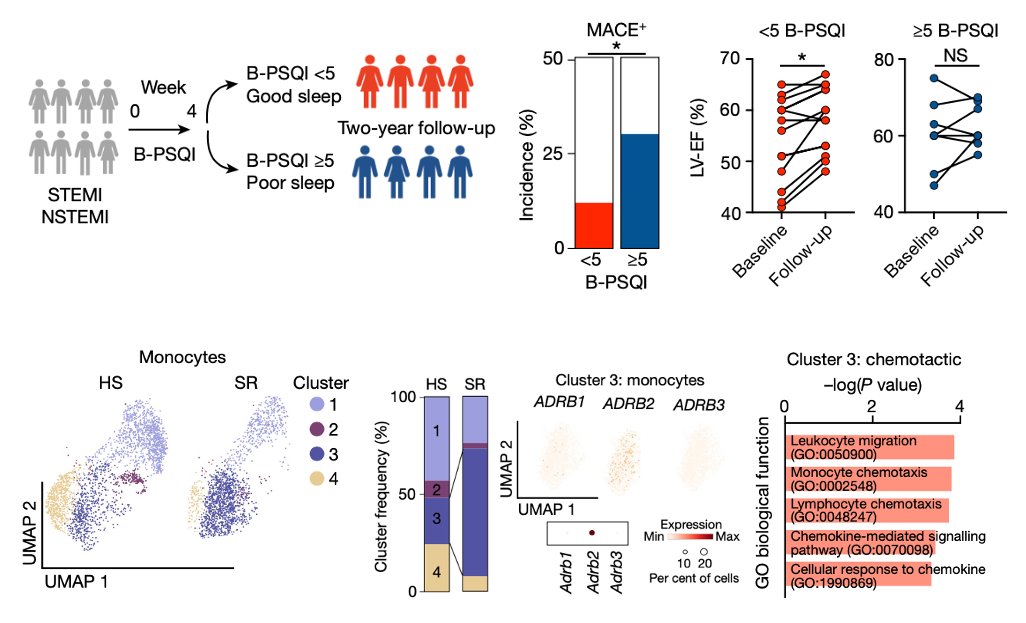
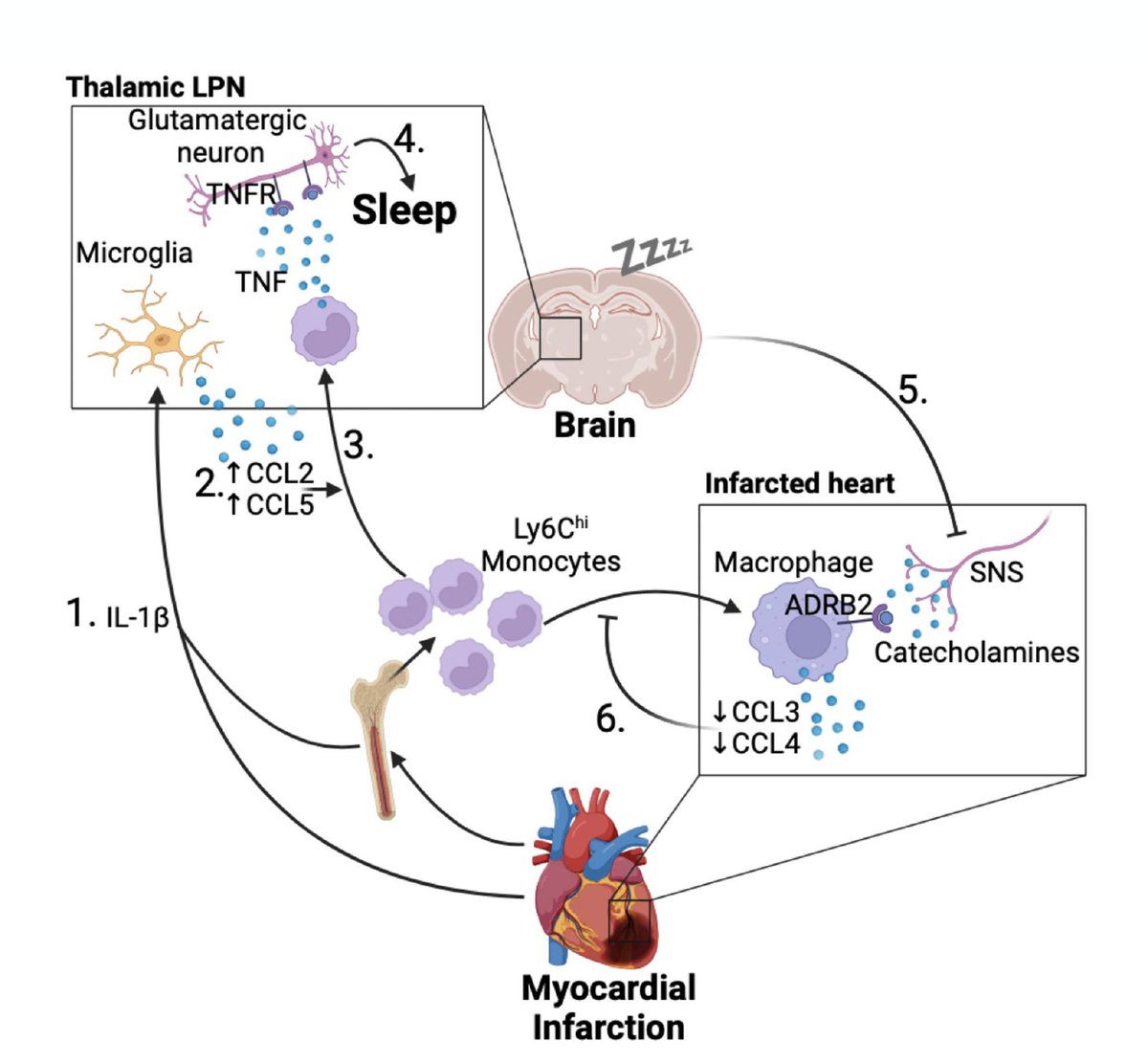
Increased sleep after MI is beneficial. In mice, fragmenting sleep after an MI worsens cardiac inflammation and damage. Sleep and TNFR1+ thalamic neurons limit sympathetic outflow from the brain to the heart, curtailing cardio-inflammation in a macrophage ADRβ2-dependent manner.
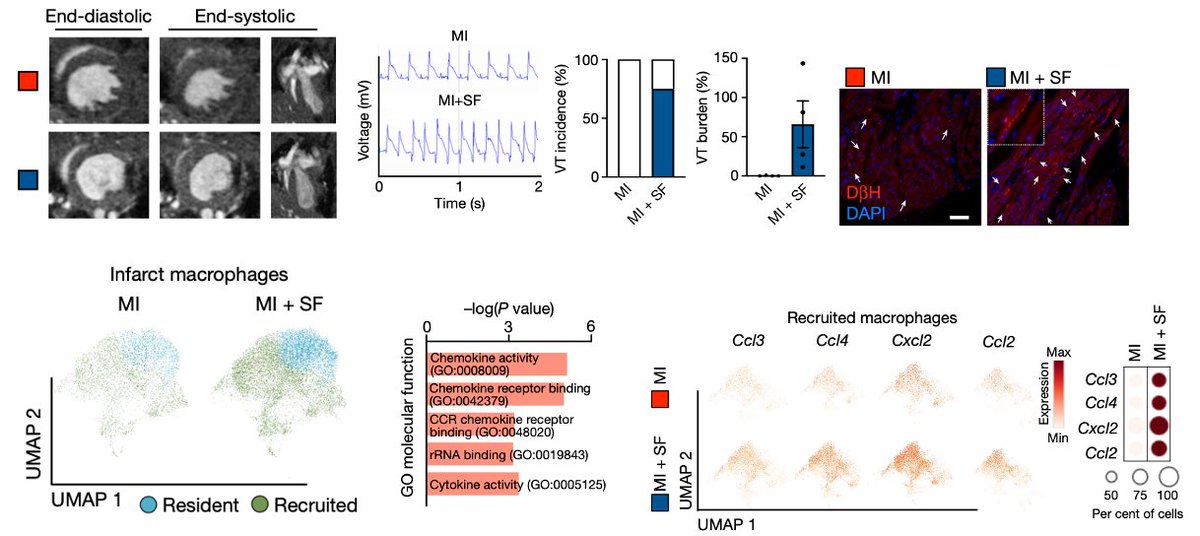
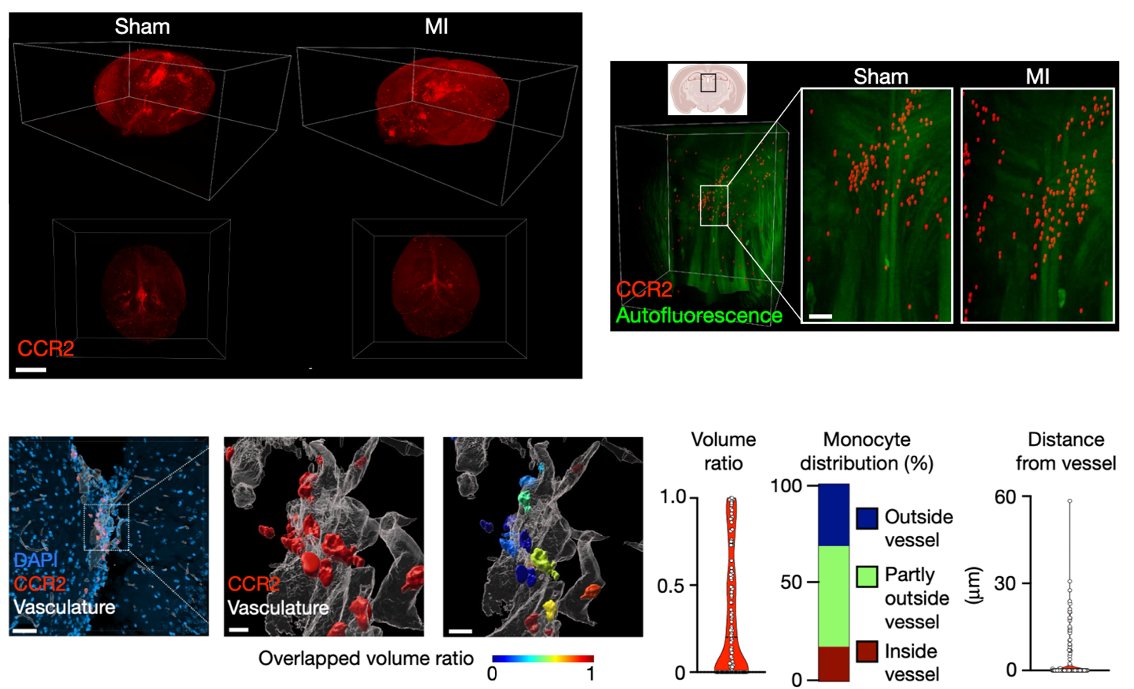
After MI, microglia recruit monocytes to the brain’s thalamus via the choroid plexus and 3ed ventricle. Once in the lateral posterior nucleus of the thalamus, monocytes gain the capacity to produce TNF which engages a subset of glutamatergic neurons to instigate a sleep circuit.
We find that atherosclerosis, heart failure, and myocardial infarction (MI) profoundly augment sleep. MI elicits a significant increase in slow wave sleep pressure, drive, and abundance after infarct. Increased SWS comes at the expense of REM and wake time. How does this happen?
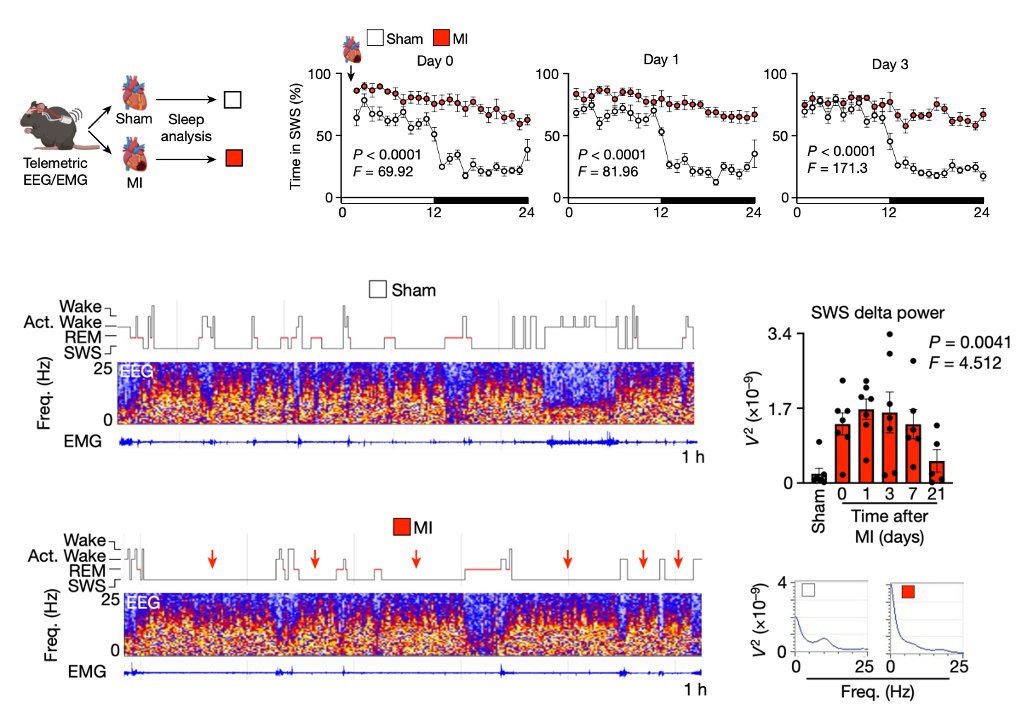
In summary, MI elicits monocyte recruitment to the brain’s thalamus to increase sleep which promotes cardiac healing and recovery. This study was driven by a fantastic lab team including Pacific, Jan, and Teresa, and would not have been possible without wonderful collaborators!

A new heart-brain-immune system discovery Following damage to the heart muscle from a heart attack, monocytes are recruited to the brain to promote sleep, limit inflammation, and healing. nature.com/articles/s4158… @peacemakerhuynh @cam_phd @IcahnMountSinai @SinaiHeartBlood…
We are delighted to share our latest findings today in @Nature We describe cardiogenic regulation of sleep after cardiac injury. “Myocardial infarction augments sleep to limit cardiac inflammation and damage” nature.com/articles/s4158…
Hideki Matsui is throwing out tonight's ceremonial first pitch!

United States Trends
- 1. $PUMP 1.797 posts
- 2. Joe and Mika 1.418 posts
- 3. Good Monday 38,7 B posts
- 4. #MorningJoe N/A
- 5. #MondayMotivation 13,2 B posts
- 6. Mika and Joe 1.548 posts
- 7. #MondayVibes 2.182 posts
- 8. Victory Monday N/A
- 9. #18Nov 1.925 posts
- 10. Bengals N/A
- 11. #MondayMood 1.596 posts
- 12. Chargers 72,5 B posts
- 13. WWIII 202 B posts
- 14. 60 Minutes 39,3 B posts
- 15. Margaret Thatcher 5.747 posts
- 16. Rusia 2.423 posts
- 17. Myron 13,3 B posts
- 18. Herbert 36,6 B posts
- 19. Brendan Carr 15,9 B posts
- 20. Burrow 40,8 B posts
Who to follow
-
 Aneesa Das, MD, FCCP, FAASM
Aneesa Das, MD, FCCP, FAASM
@AneesaDas -
 AASM Membership
AASM Membership
@AASMmembership -
 Atul Malhotra, MD
Atul Malhotra, MD
@AtulMalhotra13 -
 AASM Foundation
AASM Foundation
@aasmfoundation -
 Cathy Goldstein, MD, MS
Cathy Goldstein, MD, MS
@cathygo_sleep -
 National Sleep Research Resource (SleepData.org)
National Sleep Research Resource (SleepData.org)
@SleepDataNSRR -
 Karin Johnson
Karin Johnson
@drsleepykarin -
 Reena Mehra MD MS
Reena Mehra MD MS
@ReenaMehra0203 -
 Sai Parthasarathy, MD
Sai Parthasarathy, MD
@sai_sparthamd -
 Oren Cohen
Oren Cohen
@OrenCohen_MD -
 S Faiz
S Faiz
@sfaiz212 -
 Women in Sleep Medicine
Women in Sleep Medicine
@womeninsleep -
 David Schulman
David Schulman
@davidschulman -
 Vaishnavi Kundel, MD, MS
Vaishnavi Kundel, MD, MS
@Vaish1986 -
 Indira 💤
Indira 💤
@sleepdocpa
Something went wrong.
Something went wrong.